Understanding Ankylosing Spondylitis: What It Is, What You Need to Know, and When to Seek Help
Ankylosing spondylitis (AS) is a chronic inflammatory disease characterized mainly by the involvement of the spine but which may also affect other joints, the eye, and, in some cases, internal organs. In fact, the term itself, “ankylosing,” means stiffening or fusing, while “spondylitis” signifies inflammation of the vertebrae. If not managed properly, this disease can result in excruciating pain, stiffness, and decreasing degrees of mobility. Understanding the important facts about the condition is very crucial for everyone.
What is Ankylosing Spondylitis?
Ankylosing spondylitis is arthritis that falls under a general group of conditions called spondyloarthritis, and it is characterized by the inflammation of the sacroiliac joints, which join the base of the spine with the pelvis. Later on, this kind of inflammation will subject vertebrae to fusion, making the spine stiff and rigid. Ankylosing spondylitis varies with regard to frequency but is assumed to affect more than hundreds, mostly manifesting itself to people around young adulthood, typically at 20 up to the age of 40.
Ankylosing Spondylitis Symptoms
Symptoms of ankylosing spondylitis usually develop gradually. Early signs typically include:
- Lower back pain and stiffness: This is often the first and most intense symptom. The pain is usually described as dull and aching, particularly worse in the morning or following inactivity. The pain tends to improve as the patient moves around or performs some physical exercises.
- Buttock pain: Pain may radiate to the buttocks and sometimes down the back of the thigh.
- Morning stiffness: Stiffness lasting for more than 30 minutes with onset in the morning is a characteristic symptom.
Other ankylosing spondylitis symptoms may start appearing over time:
- Pain and stiffness extending up into the spine: Eventually, the inflammation can progress into the mid and upper back or even the neck.
- Fatigue: Constant tiredness is another prevalent complaint.
- Pain in other joints: Other joints too can be involved, such as hips, knees, shoulders, and ankles.
- Enthesitis: Pain at sites of tendon and ligament insertion onto bone, e.g., at the heel (Achilles tendonitis) or in the front of the shin.
- Chest pain: Inflammation of the joints between ribs and breastbone can lead to chest pain and difficulty taking deep breaths.
- Eye inflammation (uveitis or iritis): Inflammation can cause eye pain, redness, blurred vision, and light sensitivity.
Signs of Ankylosing Spondylitis
The following signs of ankylosing spondylitis are sought by healthcare professionals during physical examination:
- Restricted mobility of the spine: Diminished movements in the lower back region, including forward bending, backward bending, and bilateral bending.
- Sacroiliac joint tenderness: It hurts when these joints are palpated.
- Reduced chest expansion: The joints between the ribs are inflamed.
- Stooped posture: Fusion of the spine may cause it to curve forward.
- Signs of inflammation in other joints: Peripheral joints may be swollen and tender and show restriction of movement.
Ankylosing Spondylitis Causes
The exact causes for ankylosing spondylitis are not completely understood, but it is believed to be a complex interaction between genetic and environmental factors.
- Genetics: There is a very strong association between the gene HLA-B27 and the risk of ankylosing spondylitis. The presence of this gene, however, does not guarantee that a person will develop the disease. Indeed, only a small number of persons with the HLA-B27 gene ever develop ankylosing spondylitis. It has also been found to run in families, indicating the involvement of other genes.
- Environmental Factors: No specific environmental factors have been clearly identified; however, some researchers suspect certain infections or other environmental factors may be responsible for the disease in those persons genetically predisposed.
Ankylosing Spondylitis Diagnosis
The diagnosis of ankylosing spondylitis is often difficult at the early stages; the ankylosing spondylitis tests primarily involve the combination of clinical evaluation, imaging studies (especially X-rays and MRI), and blood tests (including inflammatory markers and HLA-B27) used to diagnose the condition.
- Medical History and Physical Examination: The doctor will ask for the details regarding the symptoms and other signs of ankylosing spondylitis, including their onset, duration, and the way the symptoms interfere. The doctor will also perform the physical examination in order to measure the reduction in spinal mobility and examine for tenderness in certain body areas.
Imaging Tests:
- X-rays: X-rays of the sacroiliac joints and spine may reveal inflammation and structural changes such as sacroiliitis or syndesmophytes. Early changes, however, may not show on X-rays.
- MRI: An MRI may assess inflammation and changes in the spine and sacroiliac joints earlier than an X-ray and thus is an important tool for early diagnosis.
Blood Tests:
- ESR and CRP: These are tests of inflammatory activity in the body. Raised levels may suggest an inflammatory condition but are not specific to AS.
- HLA-B27 Genetic Test: A blood test to check for the presence of the HLA-B27 gene. This gene is present in a large proportion of AS patients; also, there are people who have it and do not have the condition. Therefore, the mere presence of the HLA-B27 gene is not diagnostic by itself; it has to be considered in conjunction with the clinical picture and imaging findings.
Ankylosing Spondylitis Treatment
Ankylosing spondylitis treatment mainly focuses on pain relief, preventing complications like spinal fusion, maintaining mobility, and enhancing quality of life, often involving a combination of treatments, such as:
Medicines:
- Non-steroidal anti-inflammatory drugs (NSAIDs) are commonly used for pain and inflammation treatment.
- TNF blockers are indicated to block inflammation-causing proteins.
- Interleukin-17 inhibitors target different inflammatory pathways.
- Janus kinase inhibitors block enzymes involved in inflammation.
- Oral corticosteroids are used for short courses, while injections target specific inflammation sites.
- Disease-modifying anti-rheumatic drugs (DMARDs) are useful for peripheral joint involvement but less effective for spinal symptoms.
Ankylosing Spondylitis Therapy:
- Physical Therapy: Considered the core of therapy for AS. It involves treatment by means of exercise aimed at maintaining flexibility, improving posture, strengthening the muscles that support the spine, and reducing stiffness.
- Occupational Therapy: The occupational therapist will empower people to adapt their activities to lessen the strain on their joints and keep up their independence.
Lifestyle Modifications:
- Regular exercise to reduce symptoms and maintain mobility.
- Maintaining good posture to prevent spinal deformities.
- Alternating heat and cold therapy to alleviate pain and stiffness.
- Quitting smoking to prevent worsening symptoms and health complications.
Surgery: Generally, surgery is rarely needed for ankylosing spondylitis; however, in cases of severe hip damage leading to joint replacement or severe spinal deformities, surgery is needed.
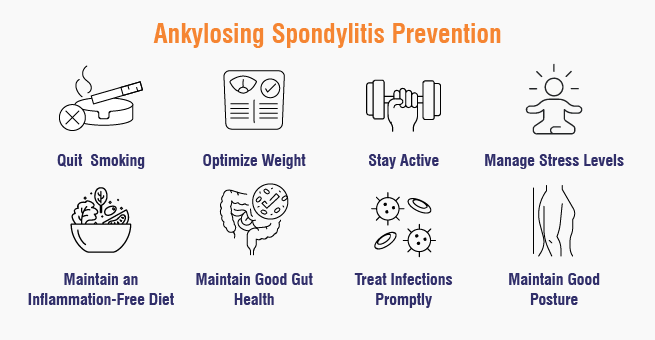
Ankylosing Spondylitis Prevention
Since the genes of a person play an important part and nothing can be done with one’s genetics, a preventive approach is not possible for the patient with ankylosing spondylitis. However, there are certain lifestyle modifications that one can try to avoid or delay triggering the condition:
- Avoid Smoking: It can increase inflammation and worsen the progression of AS. From a health standpoint, avoiding the use of tobacco should be considered. It can very well decrease the risk or make the condition less severe.
- Maintain a Healthy Weight: Being overweight places greater mechanical stress on the joints and may also contribute to inflammation. Through a balanced diet and exercise program, maintain your ideal weight.
- Try to Maintain an Inflammation-Free Diet: This can indirectly prevent AS, although this kind of diet can contain omega-3 fatty acids and many fruits, vegetables, and whole grains to help reduce the body’s overall inflammation.
- Good Gut Health: Research is finding increasing evidence that gut bacteria might be linked to autoimmune diseases. Eating an array of foods that are high in fiber as well as probiotic sources could encourage a healthy gut microbiome.
- Treat Infection Quickly: There are some hypotheses that infections can trigger the onset of AS in genetically predisposed individuals. It may therefore be important to treat infections promptly and effectively.
- Maintain Good Posture and Body Mechanics: While AS occurs internally within the spine, adopting good posture and good body mechanics in daily life activities may lessen spine strain.
- Regular Exercise and Movement: The regular practice of gentle exercises keeps the joints free and flexible, which might help even before AS has come into existence.
- Manage Stress Levels: Getting into an episode of stress would add to inflammation in the body. So anyway, stress relief may help enhance immune function.
- Consider Vitamin D Levels: Some research discusses deficiency of vitamin D in the development of autoimmune conditions. Ensuring an optimal level of vitamin D could prove beneficial.
- Know the Family History and Early Symptoms: Having a family history of AS would require one to pay close attention to particular early symptoms. Early diagnosis and treatment might slow down the progression.
When to Consult the Doctor?
One should seek the medical appointment if experiencing any of the following:
- Persistent low back pain: Especially if it’s chronic (lasting over 3 months)
- Morning stiffness: Stiffness lasting longer than 30 minutes
- Pain improves with exercise, unlike typical mechanical back pain
- Pain in buttocks/hips: Radiating pain is a red flag
- Family history of AS: Increased risk warrants earlier consultation
- Eye pain/redness: Could indicate uveitis, linked to AS
Conclusion
Taking care of ankylosing spondylitis is a never-ending task demanding an extra dose of management and calm persistence through life’s challenges. If treatment is given properly and if self-care is done diligently, many living with ankylosing spondylitis renew the opportunity of a satisfied life, being active and fulfilled.
Yashoda Hospitals has a multidisciplinary approach with skilled rheumatologists, physical therapists, and other experts to provide complete therapy for ankylosing spondylitis. In order to precisely diagnose the illness and create customized treatment programs, we provide cutting-edge diagnostic procedures. Managing symptoms, delaying the course of the illness, and enhancing the patient’s quality of life are our objectives.
Have any questions or concerns about your health? We’re here to help! Call us at +918065906165 for expert advice and support.
















 Appointment
Appointment WhatsApp
WhatsApp Call
Call More
More