Is It Myositis? Recognizing the Signs of Muscle Inflammation
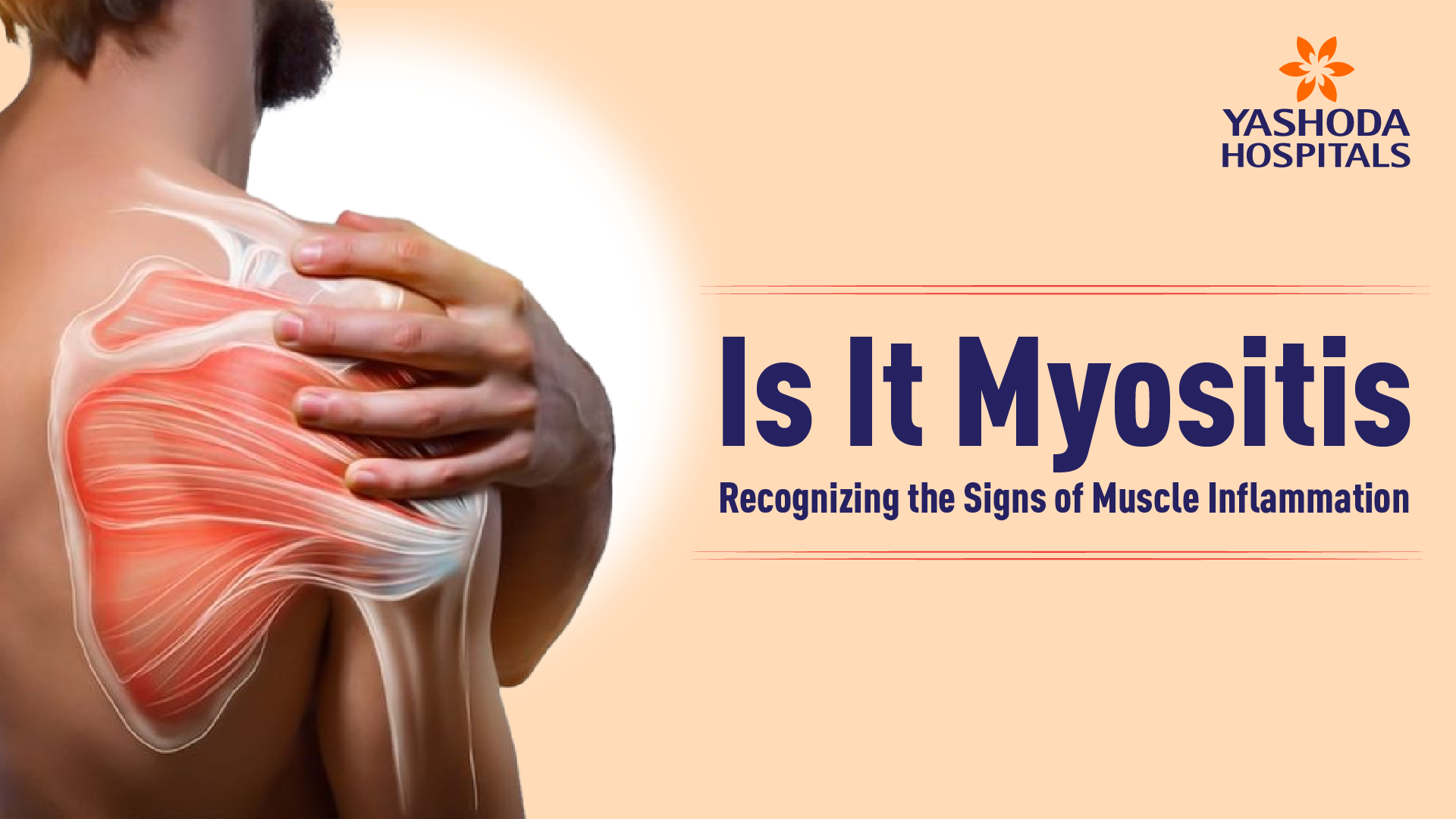
Although it happens infrequently, myositis is a term used to characterize any muscle inflammation that is associated with serious autoimmune diseases that cause persistent muscle inflammation, weakness, and pain. Many aspects of myositis, including its types, symptoms, causes, complex diagnosis, and evolving treatment concepts, are essential for early diagnosis, appropriate management, and better living conditions for those afflicted.
What is Myositis?
Myositis is a rare autoimmune condition with inflammation of the muscles, causing weakness that worsens over time. It results from an abnormal immune response in which the immune system attacks healthy muscle tissues. The inflammation is mostly localized to the proximal muscles of the limbs and trunk but may extend to other sites such as the skin, joints, lungs, and esophagus. The effect may vary from mild pain to disabling disability, all stressing the importance of timely diagnosis and adequate management.
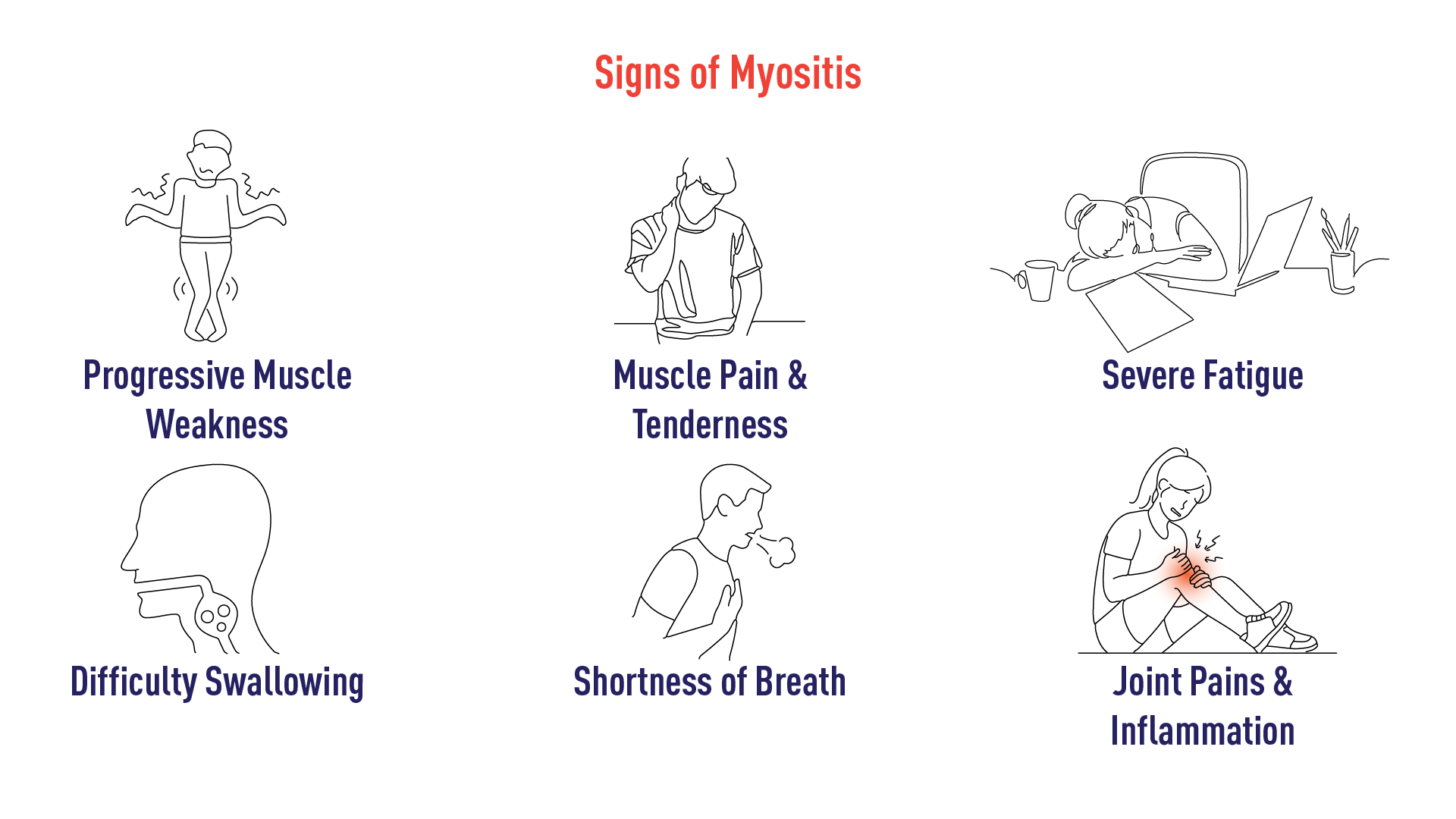
Myositis Symptoms: Recognising the Signs of Myositis
In terms of symptoms, myositis can manifest quite differently depending on the particular type of myositis and the individual patient. Some very general and characteristic symptoms are considered common:
- Progressive Muscle Weakness: This represents the hallmark of the majority of myositis types. Muscle weakness creeps in slowly—across several weeks, months, or even years—and often affects both sides of the body. Difficulty rising from a chair, climbing stairs, lifting objects, or reaching overhead is typical.
- Muscle Pain and Tenderness: Although muscle pain (myalgia) and tenderness may not occur in every case, they may be present in some forms of myositis, with levels of pain ranging from mild to severe.
- Fatigue: A shockingly consistent feature reported in many of those suffering from myositis is a persistent and debilitating fatigue, even when the levels of muscle weakness are not yet at high extremes.
- Difficulty Swallowing (Dysphagia): Inflammation of the esophageal muscles is capable of damaging them and causes difficulty in swallowing solid food or liquids, thereby increasing the risk of aspiration.
- Shortness of Breath (Dyspnea): Lung involvement known as interstitial lung disease (ILD) occurs in some myositis types.This causes shortness of breath, dry cough, and progressive lung scarring.
- Skin Rashes: Certain myositis, such as dermatomyositis, are associated with characteristic skin rashes that can precede, coincide with, or follow muscle weakness. Such rashes frequently appear on the face, including eyelids and cheeks, knuckles, elbows, knees, and chest.
- Joint Pain and Inflammation (Arthralgia and Arthritis): Not the most characteristic feature, but joint pain and inflammation may be present, especially in polymyositis and dermatomyositis.
- Raynaud’s Phenomenon: Certain people with myositis, particularly those with comorbid connective tissue disease, can get Raynaud’s phenomenon, with the toes and fingers turning white or blue on exposure to cold or stress.
- Voice Changes: Weakness of the throat muscles can lead to a hoarse or nasal voice.
Myositis Types
The “types of myositis” refer to a number of distinct autoimmune muscle disorders, each with its own distinctive features, clinical presentation, and associated conditions:
- Polymyositis (PM): Essentially involves the muscles, leading to progressive muscle weakness, usually in the proximal muscles. Pure polymyositis lacks skin rashes.
- Dermatomyositis (DM): Involves both muscle inflammation and characteristic skin rashes. The muscle weakness is the same as in polymyositis, and the rashes are variable in appearance and location.
- Inclusion Body Myositis (IBM): A slowly progressive form of myositis typically affecting older adults. It is characterized by weakness of the finger flexors and quadriceps muscles, making it hard to grip and stand up from a chair. Dysphagia is also prevalent. IBM is usually less sensitive to conventional immunosuppressive therapy.
- Juvenile Myositis (JM): A collection of rare inflammatory muscle conditions found in children and teenagers. The most prevalent form is juvenile dermatomyositis (JDM), with symptoms of muscle weakness and typical skin rashes. Juvenile polymyositis (JPM) is less prevalent and does not include the skin.
- Immune-Mediated Necrotizing Myopathy (IMNM): A newly defined subtype that involves severe weakness of muscles and muscle fiber necrosis (death) on muscle biopsy. It tends to be found with antibodies against signal recognition particle (SRP) or 3-hydroxy-3-methylglutaryl-coenzyme A reductase (HMGCR).
- Overlap Myositis: When a patient has manifestations of myositis in combination with manifestations of another connective tissue disease, e.g., scleroderma, lupus, or rheumatoid arthritis.
Myositis Causes
There is no exact cause that promotes the myositis, but it might be caused by
- Genetic Predisposition: Certain genes may predispose a person to develop an autoimmune disorder, myositis being one of these. However, people do not view myositis as a classical inheritable disorder.
- Environmental Triggers: Viral infections, some drugs (statins may induce certain cases of IMNM), and environmental toxins have been purported to be the environmental triggers in genetically susceptible individuals.
- Immune Abnormality: Essentially, the abnormality lies just within the immune system, producing autoantibodies (i.e., antibodies directed against self-antigens) and immune cells attacking muscle tissue.
- Association with Other Autoimmune Diseases: Sometimes myositis is associated with other autoimmune disorders, implying a common basis for immune mechanisms.
Myositis Diagnosis
The process of diagnosing myositis usually involves the integration of clinical assessment, laboratory investigations, and specialist tests.
- Clinical Assessment: It is important to have a complete medical history, starting with a comprehensive description of the patient’s symptoms of myositis, the onset of these symptoms, their progression, and any accompaniment of additional symptoms. A physical examination will be done in order to assess the muscle strength, reflexes, and skin signs.
- Blood Tests: Few blood tests can aid in the diagnosis of myositis:
- Specific autoantibodies like anti-Jo-1, anti-SRP, anti-Mi-2, and anti-MDA5 aid in diagnosis and classification.
- Elevated levels of muscle enzymes like creatine kinase (CK) indicate muscle damage.
- Elevated erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP) indicate inflammation, not specific to myositis.
- Nerve Conduction Studies (NCS): These are done in combination with EMG to exclude nerve disease that may cause muscle weakness.
- Electromyography (EMG): EMG evaluates muscle electrical activity and may reveal patterns of muscle inflammation and injury.
- Muscle Biopsy: A muscle biopsy, where tissue is removed surgically and inspected under a microscope, is usually the diagnostic test of choice for myositis. Muscle tissue removed by biopsy can show typical findings of inflammation, injury, and the deposition of certain proteins or inclusions, which allow the myositis to be classified by type.
- Imaging Tests: Magnetic resonance imaging (MRI) of the muscles can be used to identify muscle inflammation and damage, to select the site of biopsy, and to determine the degree of muscle involvement. Chest X-rays or CT scans can be employed to screen for lung disease (ILD).
Myositis Treatment
The primary goals of myositis treatment are to reduce inflammation in the muscle and improve muscle strength and function. Myositis treatments often comprise a combination of medication and therapies:
- Corticosteroids: These are generally indicated to reduce the muscle inflammation and the pain.
- Immunosuppressants: The immunosuppressant medications, besides corticosteroids, are usually used in the operation of controlling an autoimmune attack or reducing the demand for corticosteroids for long periods.
- Intravenous Immunoglobulin (IVIg): IVIg is a mixture of antibodies prepared from healthy donors and can work well in some types of myositis, particularly dermatomyositis and IMNM.
- Biologic Agents: In some refractory situations, biologics that target specific immune elements may be used.
- Physical Therapy: Physical therapy is essential in maintaining and improving muscle strength and flexibility, as well as range of motion. Exercises are built around the individuals’ capabilities and progress accordingly.
- Occupational Therapy: Occupational therapists can assist individuals in modifying daily activities to conserve energy and cope with muscle weakness by substituting devices and techniques to stay independent.
- Speech Therapy: When swallowing difficulties occur, this therapy helps improve swallowing function and reduces the odds of aspiration.
- Pulmonary Rehabilitation: These are the pulmonary rehabilitation programs for those with lung involvement (ILD) to improve breathing and exercise tolerance.
- Pain Management: Management will include muscle or joint pain using medicines, heat or cold therapy, or supportive treatments.
The specific myositis treatments will be based upon the types of myositis, their severity, the response to therapy from that individual, and any complications associated with it.
Lifestyle Modifications: Living Well with Myositis
Myositis medications and therapies will always be among the first things to address; yet lifestyle changes will empower one to ease their symptoms and tend to their well-being. Here are some important tips about lifestyle changes for myositis patients:
- Rest: Very often, myositis brings along excessive fatigue. Make sure you have your rest periods planned throughout the day, and learn to pace yourself. Attune to your body; it will tell you when to stop.
- Gentle Exercise as Tolerated: Strenuous exercise exacerbates muscle inflammations. However, very helpful low-impact exercises include walking, swimming, or aqua aerobics for muscle strength, flexibility, and cardiovascular function. Consult with your doctor or physical therapist before starting any new exercise routines.
- Eat a Healthy and Anti-Inflammatory Diet: A nutrient-rich diet with lots of fruits, vegetables, whole grains, and lean protein is one to aim for. Also, foods with anti-inflammatory properties, like fish with omega-3 oils and flaxseeds, may provide help.
- Water Intake: Proper hydration aids health and prevents cramping and fatigue in muscles. Always have a glass bottle of water nearby, and keep sipping during the day.
- Manage Stress Well: Chronic stress aggravates inflammation and fatigue. With this in mind, prepare to work on relaxation practices such as yoga, meditation, and more.
- Adequate Sleep: Quality sleep is crucial to allow muscle repair and overall good health.
- Protecting Skin: Avoid sun exposure to the skin by wearing suitable protective clothing, a sun hat, and sunscreen if one has dermatomyositis, as sunlight tends to aggravate the skin rash.
- Maintain an Ideal Weight: Excess weight stresses already weak muscles and joints. Try to stay in your ideal weight range through a balanced diet and suitable exercises.
- Avoid Known Triggers: Some people may notice that some activities, foods, or environmental factors seem to aggravate their myositis symptoms. Be attentive to the body and try to avoid any of these identified triggers.
When to Seek Medical Assistance?
One should consult the doctor if experiencing any of the following:
- progressive muscle weakness
- Unexplained muscle pain
- Significant fatigue
- Skin rash with muscle weakness
- Symptoms not improving
- Any sudden, severe muscle symptoms
Conclusion
Timely recognition based on diligent examination, laboratory investigation, and correct diagnosis is very crucial. Although there is not yet a cure, a multidisciplinary approach including medications, therapies, and supportive care seeks to control inflammation, maintain muscle function, relieve symptoms, and eventually enhance the quality of life for those afflicted with this debilitating disease. Future treatments hold hope in ongoing research for more effective and targeted therapy.
Yashoda Hospitals provides comprehensive care for individuals affected by myositis. Our experienced rheumatologists and multidisciplinary team offer advanced diagnostic capabilities to accurately identify the specific type of myositis. Treatment plans are tailored to each patient’s unique needs, incorporating appropriate medications, rehabilitation services, and supportive therapies. With a patient-centric approach, Yashoda Hospitals strives to effectively manage myositis, alleviate symptoms, and enhance the well-being of those under their care.
Have any questions or concerns about your health? We’re here to help! Call us at +918065906165 for expert advice and support.
















 Appointment
Appointment WhatsApp
WhatsApp Call
Call More
More