COPD Explained: What It Is, When to Worry, and When to See a Doctor
Chronic Obstructive Pulmonary Disease (COPD) is a progressive disease that obstructs airflow and contributes to substantial morbidity and mortality worldwide, including in India. Traditional risk factors such as smoking and biomass fuel exposure, along with steadily rising air pollution, put a substantial number of people at risk. It is essential for individuals, families, and healthcare practitioners to understand COPD disease: its causes, symptoms, diagnostic methods, and steps in treatment.
What is COPD?
COPD essentially represents a collection of progressive lung disorders that create airflow blockage, making it harder to breathe. Unlike acute respiratory diseases, COPD is expected to represent long-lasting breathing problems and airflow obstruction. It is a highly preventable and treatable disease but is not curable. Most of the damaging aspects of COPD are irreversible, but that damage usually worsens over time.
The two specific conditions lumped together to describe COPD are
- Chronic Bronchitis: This condition results from inflammation and swelling of the bronchial tubes (the tubes that carry air to and from the lungs), resulting in a cough productive of mucus (sputum) for at least three months a year for two consecutive years.
- Emphysema: This is a progressive process that gradually destroys the air sacs (alveoli) of the lungs, causing less elasticity and rupturing within the lungs. Once the thin walls of the air sacs are destroyed, the air leaves behind larger, less effective air spaces in the lungs, therefore getting less surface area for oxygen absorption.
COPD patients often experience persistent airflow limitations, despite various disease processes, making it a common thread among all COPD patients.
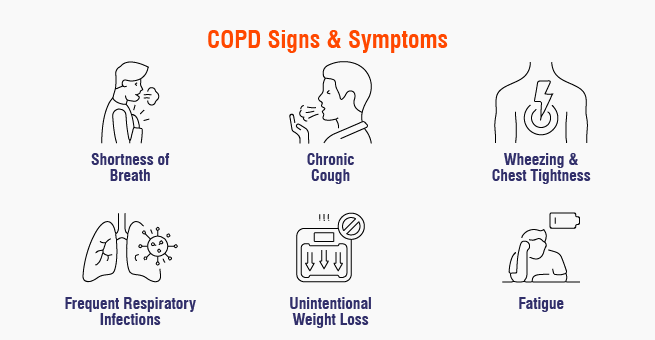
Recognizing the Signs: COPD Symptoms
In most cases, the symptoms of COPD develop slowly and worsen over time. Most people who have COPD begin to experience early symptoms but often dismiss these symptoms as “aging” or the effects of past smoking (or both). This delay can meaningfully postpone diagnosis and treatment. Some common symptoms of COPD include
- Shortness of Breath (Dyspnea): The hallmark symptom of COPD is shortness of breath. Patients with COPD often experience this symptom, particularly with physical activity. A person with COPD may experience dyspnea before the disease has significantly impacted their quality of life. For example, in the early stage of disease, a person may only experience shortness of breath while exerting themselves purposely (e.g., running), but as the condition worsens, it can occur with minimal exertion or even at rest (which would indicate advanced disease).
- Chronic Cough: A chronic cough is quite common in COPD. Many people might describe their chronic cough as a “smoker’s cough.” The cough may be dry or produce sputum that can be clear, white, yellow, or greenish.
- Wheezing: Wheezing is a whistling or squeaky sound when breathing—it is often caused by the narrowing of the airways.
- Chest Tightness: This term describes a feeling of pressure or tightness in the chest.
- Frequent Respiratory Infections: COPD patients are more likely to get colds, the flu, or pneumonia, which can dramatically reduce their lung function.
- Fatigue: Fatigue can be caused by low oxygen levels and because of the effort breathing takes.
- Unintentional Weight Loss: In the more advanced disease stages, the effort of breathing may burn significant calories, leading to weight loss.
- Swollen Ankles, Feet, and/or Legs (Edema): Advanced COPD may lead to swollen ankles, feet, or legs if the heart is involved (cor pulmonale).
- Bluish Lips or Nail Beds (Cyanosis): This indicates critically low levels of oxygen. This indicates very severe disease.
Patients may experience any of these symptoms to different extents, and each may correlate with the stage of the disease. “Exacerbations” (flare-ups) are episodes characterized by a sudden worsening of symptoms, at times requiring urgent medical care.
COPD Causes: What Causes COPD?
Most of the causes of COPD are associated with long-term congestion of lung irritants. The most common cause is as follows:
- Tobacco Smoking: This is the most common cause of both active and passive destructive lung irritants. Tobacco smoke actively irritates and inflames your airways, destroys the elastic fibers in the lungs, and damages the cilia (tiny hair-like structures that help sweep mucus out of the airway).
In addition to tobacco smoke, other important causes of COPD are
1. Outdoor Air Pollution: Long-term exposure to air pollution in the environment, mainly fine particulates and ground-level ozone, can lead to the development of COPD.
2. Occupational Dusts and Chemicals: Various dusts (e.g., coal dust, silica, cadmium) and chemicals (e.g., isocyanates, fumes) in the workplace can increase the risk of developing COPD, especially if proper precautions are not in place.
3. Indoor Air Pollution: Due to lack of options, especially in parts of the world that are developing, indoor air pollution from burning biomass fuels (wood, animal dung, and crop residue) for cooking and heating can be the cause of COPD in poorly ventilated homes.
4. Genetic Predisposition: Although one rare genetic condition, Alpha-1 Antitrypsin (AAT) deficiency, is less common than the other causes of COPD, it is an important one. Alpha-1 antitrypsin is a protein in the lungs that protects them from damage; those with AAT deficiency have a sensitivity to lung damage even if they don’t expose themselves to significant amounts of smoke.
5. Asthma and Airway Hyperresponsiveness: While asthma is not COPD, some individuals with severe, chronic asthma might develop airflow limitation, or severity that may not be fully reversible after treatment, limited in the sense that they will still fall under the definition of COPD. Another term for this overlap between asthma and COPD is “asthma-COPD overlap syndrome.”
6. Prior Childhood Respiratory Infections: The potential impact of suffering repeated, severe respiratory infections during childhood on lung function may be significant and is related to a continued increased risk of developing COPD as an adult.
Note: COPD typically develops over several years, with symptoms becoming more noticeable as lung damage worsens.
COPD Diagnosis: How is COPD Diagnosed?
Diagnosing COPD involves a combination of medical history, physical exam, and tests for lung function. The evaluation will typically include
- Medical History: The doctor will ask questions about your smoking history, history of exposure to occupational dusts or chemicals, family history of lung disease, and your symptoms, including how long you’ve had them.
- Physical Examination: The doctor can’t diagnose COPD with physical examination alone but can see signs of wheezing, prolonged exhalation, or barrel chest due to overinflation of the lungs.
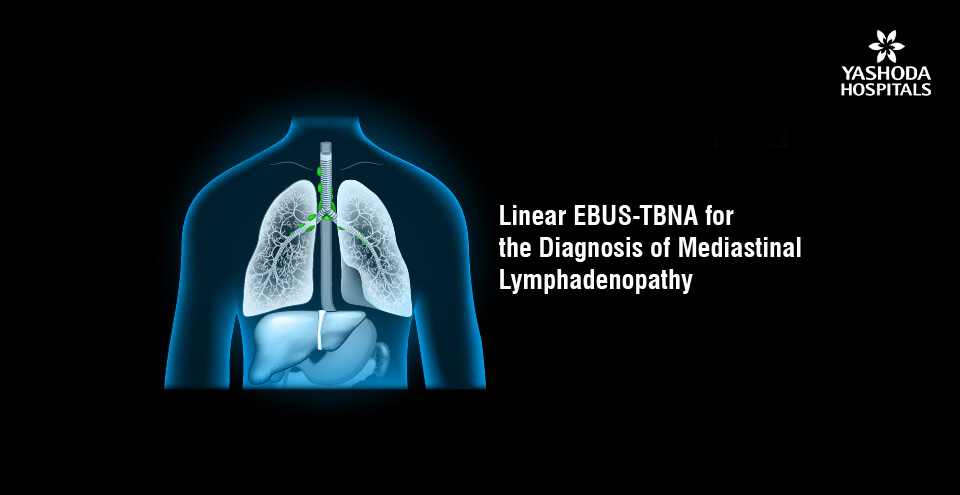
- Spirometry: This is the gold standard for COPD diagnosis. Spirometry measures how much air you can blow out and how quickly by a simple, noninvasive lung function test.
You blow as hard and fast as you can into a device called a spirometer after having a deep breath. The key measurements for diagnosis are
-
- Forced Vital Capacity (FVC): The total amount of air you can blow out after a deep breath.
- Forced expiratory volume in 1 second (FEV1): The amount of air you can blow out in the first second. A ratio of FEV1/FVC less than 0.70 (or 70%) after bronchodilator is indicative of airflow limitation and is consistent with COPD. The lower the FEV1, the greater the severity of the airflow obstruction.
After spirometry, a healthcare provider may have other tests to better assess the condition or rule out different diseases:
- Chest X-ray: A COPD X-ray can not actually diagnose COPD. Early changes may not appear on a chest x-ray. However, chest X-rays may be useful to help rule out other lung conditions like pneumonia, heart failure, or lung cancer. If a person has advanced emphysema, a chest x-ray might show hyperinflation or flat diaphragms.
- CT Scan of the Chest: A CT scan (or “cat scan”) of the chest is a more comprehensive imaging test than an x-ray and can provide sharper pictures of the lungs and is able to identify emphysema and possibly bronchiectasis (also a chronic lung condition). A CT scan may also be used to screen for lung cancer, especially if you are at high risk for lung cancer.
- Arterial Blood Gas (ABG): This is a test done to measure the quantity of oxygen and carbon dioxide in your blood and shows your lungs’ ability to obtain oxygen and dispose of waste gases.
- Alpha-1 Antitrypsin Deficiency Test: For those who are too early for the diagnosis of COPD, have a family history of COPD, or have COPD that doesn’t follow normal risk factor patterns, this test is recommended.
A complete diagnostic process is vital to achieve the accurate diagnosis of COPD and develop an appropriate treatment plan.
COPD Treatment & Management
Although there is currently no cure for COPD, COPD management and COPD treatment can greatly relieve symptoms, enhance quality of life, reduce the number and severity of exacerbations, and slow the aggravation of disease.
1. Smoking Cessation: The Most Important Step
If you are a current smoker, quitting smoking is the most important and effectual step of COPD management. Quitting smoking can not only slow the rate of decline of lung function, reduce symptoms, and decrease the risk of exacerbations but also facilitate maintaining better overall health. There are many ways to quit smoking with many different types of support mechanisms, such as nicotine replacement therapy, medications, and behavioral therapy.
2. COPD Medications
The medications used to treat COPD focus on making the airways open, lowering the level of inflammation, and preventing flare-ups. These medications are usually given in an inhaler, which allows the medication to go directly into the lungs.
Bronchodilators: Bronchodilators are medications that relax the muscles surrounding the airways and open them up to make breathing easier.
- Short-Acting Bronchodilators (SABAs): Short-acting bronchodilator medications provide fast relief of symptoms in a situation of flare-ups.
- Long-Acting Bronchodilators (LABAs): Long-acting bronchodilator medications provide long-lasting bronchodilation. These medications are taken regularly every day to prevent symptoms.
- Long-Acting Muscarinic Antagonists (LAMAs): An additional family of long-acting bronchodilators that work slightly differently than LABAs but are also very effective. These medications can be taken with LABAs for dual-action bronchodilation.
Most often, one would get a LABA and a LAMA together as a treatment to get a better effect.
- Inhaled Corticosteroids (ICS): Inhaled corticosteroid medications reduce the inflammation in the airways. ICS medications are usually used with LABA medications in patients with frequent exacerbations or with features of asthma-COPD overlap.
- Combination Inhalers: Many inhalers contain combinations of a LABA, an ICS, or a LABA, LAMA, and ICS medications that are easier to use.
- Oral Corticosteroids: Oral corticosteroids are used for very short periods during acute exacerbations to help reduce. Long-term oral corticosteroid therapy is usually avoided.
- Phosphodiesterase-4 (PDE4) Inhibitors: These can be used in severe COPD with chronic bronchitis and with a background of exacerbations in order to decrease inflammation and relax airways.
- Antibiotics: These are prescribed during bacterial exacerbations of COPD to eliminate the infection.
- Oxygen Therapy: For patients with severe COPD and low blood oxygen levels (hypoxemia), supplemental oxygen has been shown to greatly improve shortness of breath, increase exercise tolerance, and decrease strain on the heart. Oxygen can be delivered via nasal prongs or a mask.
3. Pulmonary Rehabilitation
Pulmonary rehabilitation is a comprehensive program aimed at improving both the physical and psychological well-being of people with chronic respiratory disease and encouraging the long-term adoption of health-enhancing behaviors. It is an important component of the COPD care plan and consists of
- Exercise Training: Customized exercise programs specifically designed to improve strength, endurance, and the efficiency of the breathing process.
- Breathing Techniques: Learning techniques such as pursed-lip breathing and diaphragmatic breathing to optimize airflow and reduce shortness of breath.
- Education: Knowledge about COPD, medication use, exacerbation management, and techniques/modifications for energy conservation.
- Nutritional Counseling: Assess and deal with issues of weight loss or weight gain when considering body weight has implications for lung function.
- Psychosocial Support: Anxiety, depression, and social isolation are common to chronic illness, and so the role of psychosocial support across the continuum of being ill to being well is important.
4. Vaccinations: Prevention of Infection
People with COPD are at an increased risk for respiratory infections and should be afforded routine vaccinations.
– Annual Flu Vaccine: To prevent infection with influenza, which can lead to serious exacerbations in COPD patients.
– Pneumococcal Vaccines: To prevent pneumonia caused by the pathogen Streptococcus pneumoniae
5. Nutrition support
Maintaining a healthy weight is an important aspect of pulmonary rehabilitation. If you are underweight, it is easy to weaken your muscles, including the muscles you use to breathe. If you are overweight, it may make breathing more difficult. Nutrition counseling would help develop a nutritional plan that is appropriate for you.
6. Treating Exacerbations
A COPD exacerbation occurs when the acute symptoms of the respiratory system worsen to the point where medication changes are required and potential hospitalization is indicated. A good plan for care will include early recognition of symptoms, a pre-established action plan, and emergency contacts for urgent medical attention.
7. Bronchoscopic Thermal Vapor Ablation (BTVA)
BTVA is a minimally invasive surgery introduced to help patients breathe better who are severely emphysematous, a component of lung disease called COPD. BTVA is performed using heated water vapor via a bronchoscope to targeted, diseased lung areas via bronchoscopy. The objective is for the vapor to cause the damaged tissue to shrink and fibrose; the total volume of lung decreases. In essence, BTVA actively shrinks diseased and overinflated parts of the lung, allowing the less damaged and healthier areas to expand more effectively and limit air trapping, which ultimately may improve pulmonary function, exercise tolerance, and quality of life in selectively chosen patients.
8. Non-invasive Ventilation (NIV) BiPAP
Non-invasive Ventilation (NIV) when using BiPAP (Bilevel Positive Airway Pressure) is a breathing support therapy that allows them to use a mask (nasal, oral, or full face) to receive pressurized air instead of the invasive tube. In COPD, BiPAP helps patients with acute exacerbations (flare-ups) when they have worsening difficulty breathing to such an extent that carbon dioxide builds up (hypercapnia) in their body and they have low oxygen. BiPAP helps patients by more easily supporting inspiration (the inhalation phase of breathing), maintaining positive pressure on expiration (which helps keep the airway open to allow for the clearance of CO₂), and reducing the overall work of breathing. BiPAP may be used non-invasively to prevent needing invasive mechanical ventilation (intubation), so it is considered a non-invasive method of ventilation. BiPAP can be used long-term in a small subset of stable COPD patients who experience chronic hypercapnia.
9. Surgical Options (Less Frequent)
In a small number of individuals with a diagnosis of severe emphysema, surgical options are a potential consideration:
- Bullectomy: Surgery to take out large, air-filled sacs (bullae) that are compressing healthy lung tissue.
- Lung Volume Reduction Surgery (LVRS): Surgery to take out the severely damaged lung so that the important and healthy parts of the lung can create more function.
- Lung Transplant: A last resort for very severe COPD only for highly selected patients.
COPD Care Plan
It is important to have a personal COPD care plan for ongoing long-term management. A personal plan should be created with the support of the healthcare team (pulmonologist, physician, respiratory therapist, dietitian, etc.) and should include
- Medication Plan: Guidelines on which COPD medications to take, when to take them, and how to take them.
- Inhaler Technique Training: Training on how to use inhalers correctly so that the most medication gets into your lungs.
- Symptom Tracking: Regular tracking of the COPD symptoms (shortness of breath, cough, and mucus production).
- Exacerbation Action Plan: Action plan of how to deal with worsening symptoms.
- Exercise Plan: Specific exercises and activities within your abilities.
- Nutrition Plan: Suggested weight management and dietary goals to maintain health.
- Vaccination Promotion: Reminders for the annual flu vaccine and pneumococcal vaccine.
- Smoking Cessation Plan: If you smoke, ongoing treatment to help you quit.
- Psychosocial Support Resources: Resources on how to cope with emotional stress and distress related to COPD.
- Regular Follow-up Appointments: Schedule appointments with the pulmonology team on a regular basis to follow up on health and adjust the plan as needed.
Lifestyle Modifications
Living with COPD has its challenges, but with an adequate COPD management plan and being proactive, it is possible to maintain a good quality of life.
- Get active: Moderate physical activity will have a positive impact on the breathing, one’s energy level, and their overall well-being; even gentle walking can make a significant difference.
- Breathing exercises: Pursed-lip breathing and diaphragmatic breathing can help us make every breath as effective as possible.
- Reduce stress: Stress and anxiety can contribute to a feeling of breathlessness. There are more and more relaxation techniques available (meditation, yoga, or different forms of deep breathing).
- Eliminate lung irritants: Don’t expose yourself to cigarette smoke or air pollutants, and maintain a safe environment at home (and in the workplace) to reduce dust.
- Keep yourself clean: Regular handwashing and avoiding crowds during flu season can minimize the chance of infections.
- Stay hydrated: Maintaining high fluid intake may be beneficial in thinning mucus and aiding in removal.
When to Seek Medical Help from a Doctor?
It is important for people with COPD to determine when to seek medical attention because symptoms can escalate quickly. Here is a guide to determine when you should contact your pulmonologist and when you should go to the emergency room. One should contact your healthcare professional if you notice changes in your usual COPD symptoms, such as
- Worsening cough: if your cough appears to be worse than usual or occurs more frequently.
- Change in mucus: if you have an increased amount of mucus or if there is any change in the mucus color (clear to yellow, green, or brown) or thickness.
- Increased shortness of breath: if you find it more difficult to breathe than usual, especially during ordinary activities. Needing to use your quick-relief inhaler more often.
- Increased wheezing: if your breathing sounds like it has become noisier or more whistling.
- Increased fatigue: if you are finding that you feel more tired than usual for more than a day.
- Trouble sleeping: if you find it more difficult to sleep than usual.
- Fever: A mild fever that does not go down.
The sooner you intervene with regard to a COPD exacerbation (flare-up), the better chance you have of preventing it from getting serious.
Conclusion
Chronic Obstructive Pulmonary Disease (COPD) is a serious condition that can be managed through understanding its symptoms, timely diagnosis, and a comprehensive care plan. By recognizing symptoms, undergoing treatment, and committing to a well-structured care plan, individuals can lead fulfilling lives. With proactive care, self-management, and healthcare support, living well with COPD can be achievable. Every step towards better lung health is a step towards a more vibrant and unhindered life.
Yashoda Hospitals in Hyderabad provides comprehensive care for COPD and related respiratory conditions. Our Center for Pulmonology and Critical Care Medicine has a team of expert pulmonologists and lung specialists, offering consultations, diagnostics, and therapeutic interventions. We manage a range of pulmonary diseases, including complex cases, severe respiratory failure, and various infections. The hospital focuses on patient-centered care using a multidisciplinary team approach to slow disease progression and improve quality of life for COPD patients.
Have any questions or concerns about your health? We’re here to help! Call us at +918065906165 for expert advice and support.










 Appointment
Appointment WhatsApp
WhatsApp Call
Call More
More