Vasculitis: Understanding the Causes, Diagnosis, and Management of Inflamed Blood Vessels
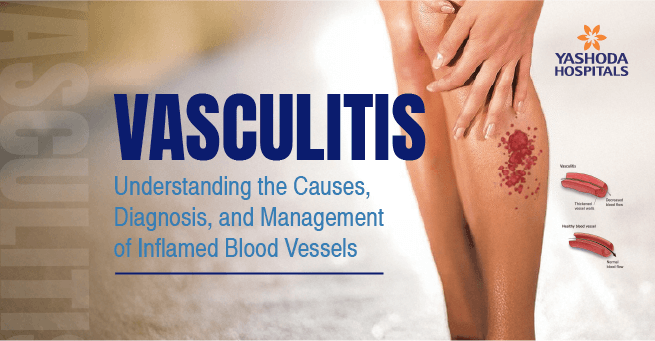
Vascular inflammation is a hallmark of a wide range of rare diseases often referred to as vasculitis. Vasculitis causes the vessel walls to thicken, narrow, weaken, or even scar, which can impair the flow of blood and might harm the body’s organs and tissues. Identifying the various vasculitis symptoms, learning about the various vasculitis types, investigating the possible vasculitis causes, comprehending the intricacies of vasculitis diagnosis, and understanding the existing vasculitis treatment options are essential for early intervention and better outcomes in patients suffering from these diseases.
What is Vasculitis?
Vasculitis is a group of conditions resulting from inflammation of blood vessels, including arteries, veins, and capillaries. In general, the circulatory network consists of arteries carrying oxygenated blood away from the heart, veins carrying deoxygenated blood back to the heart, and capillaries facilitating blood-to-tissue exchange. Inflammation of these circulatory blood vessels can cause thickening, narrowing, weakening, or scarring, reducing blood flow and causing damage to tissues and organs that rely on these vessels for oxygen and nutrients. Inflammation can cause widespread and varied consequences, including aneurysms, rupture, and internal bleeding. Vasculitis can occur independently (primary vasculitis) or be triggered by other conditions like infections, autoimmune diseases, certain medications, or certain types of cancer (secondary vasculitis).
Vasculitis Types
Some of the major vasculitis types include
- Large Vessel Vasculitis: It mostly affects the aorta and its main branches. This group includes
- Giant Cell Arteritis (GCA): GCA affects individuals over 50, causing headache, scalp tenderness, jaw pain, and vision loss.
- Takayasu’s Arteritis: Takayasu’s Arteritis affects individuals under 50, causing arm or leg claudication, absent pulses, and organ damage.
- Medium Vessel Vasculitis: Primarily affects medium-sized arteries that nourish organs and tissues. This group includes
- Small Vessel Vasculitis: It mostly affects the tiny arteries, arterioles, capillaries, and venules. This group includes
- Granulomatosis with Polyangiitis (GPA): Often affects upper and lower respiratory tracts and kidneys.
- Microscopic Polyangiitis (MPA): Commonly affects kidneys and lungs.
- Eosinophilic Granulomatosis with Polyangiitis (EGPA): Characterized by asthma, high eosinophil levels, and organ involvement.
- Immune Complex Small Vessel Vasculitis: Involves the deposition of immune complexes in small blood vessels. This group includes
- Henoch-Schönlein Purpura (HSP) affects predominantly children.
- Cryoglobulinemic Vasculitis linked to hepatitis C infection.
- Hypersensitivity vasculitis, which is triggered by medications, infections, or antigens.
Vasculitis Causes
The specific vasculitis causes are usually unknown (idiopathic). Nevertheless, in most instances, the underlying mechanism is a dysregulation of the immune system. Various factors are thought to be responsible for the onset of vasculitis:
- Autoimmune Disorders: Most types of vasculitis are autoimmune disorders, in which the immune system creates autoantibodies and immune cells that attack blood vessel components.
- Genetic Predisposition: There are some genetic factors that can predispose a person to developing vasculitis, though it is usually not inherited directly.
- Infections: Certain infections, including hepatitis B, hepatitis C, and streptococcal infections, have been associated with the development of some types of vasculitis.
- Medications: Specific medications are responsible for hypersensitivity vasculitis in a minority of individuals.
- Cancer: In very infrequent situations, vasculitis is found together with occult cancers.
- Environmental Triggers: Exposure to environmental irritants or causes is less specific but perhaps etiologic.
Vasculitis Symptoms
The vasculitis signs are enormously variable and are very likely to simulate those of countless other ailments, frequently creating difficulties in establishing early diagnosis. The individual signs someone develops rely on which of their blood vessels have been targeted by the illness and which organs the affected vessels service. There are some widespread and generalized signs of vasculitis, such as
- Fever: Often unremitting and unexplained.
- Fatigue: Extreme and profound tiredness.
- Weight loss: Unintended and significant.
- Pain: Muscle pains (myalgia) and joint pain (arthralgia): distributed or localized.
- Skin rashes: Varied in appearance, such as small red spots (petechiae), larger bruises (purpura), nodules, or ulcers.
- Nerve issues: Numbness, tingling, weakness, or pain in the limbs (peripheral neuropathy).
- Headaches: Might be severe or persistent.
- Vision changes: Blurred vision, double vision, or eye pain.
In addition to these above symptoms, direct organ involvement can cause a broad spectrum of additional manifestations:
- Kidneys: Hematuria (blood in the urine), proteinuria (protein in the urine), and renal failure.
- Lungs: Dyspnea (shortness of breath), cough, and possible lung injury.
- Gastrointestinal tract: Abdominal discomfort, nausea, vomiting, and bleeding.
- Heart: Pain in the chest, dyspnea, and possible myocardial infarction or heart failure.
- Brain: Stroke, seizures, or mental impairment.
- Ears, nose, and throat: Sinusitis, nasal bleeding, loss of hearing, and mouth or nasal ulcers.
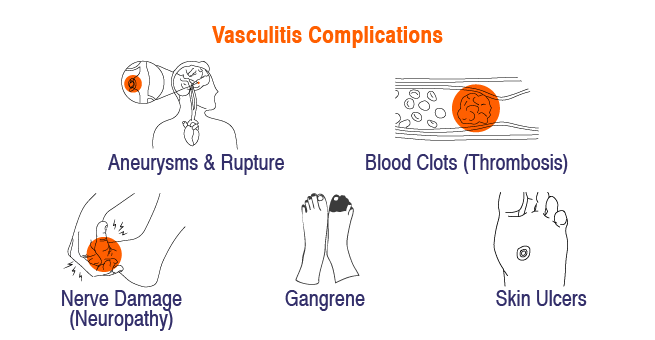
Vasculitis Complications
Vasculitis, which is the inflammation of blood vessels, in some rare cases can create a host of complications based on the type and severity of vasculitis and which organs are affected. The following are some of the possible main complications:
- Organ Damage: Decreased blood flow as a result of inflamed or narrowed vessels can cause ischemia (lack of oxygen), which can significantly damage vital organs, such as the kidneys, lungs, heart, and brain.
- Aneurysms and Rupture: When the walls of a blood vessel become weak, bulging can occur, or an aneurysm, which can rupture and result in internal bleeding and possibly life-ending situations.
- Blood Clots (Thrombosis): The inflammatory process increases thrombosis by impacting the vessels, which can result in the clot and might cause deep vein thrombosis or pulmonary embolism.
- Nerve Damage (Neuropathy): Vasculitis can impact the vessels supplying blood to nerves, causing nerve damage, which produces numbness, tingling, pain, and weakness.
- Skin Ulcers and Gangrene: Lack of blood supply to the skin can lead to painful ulceration, and in extreme cases, medical intervention is needed for tissue death (gangrene).
Vasculitis Diagnosis
The vasculitis diagnosis may be difficult because these diseases are rare and share overlapping symptoms with other illnesses. A careful and methodical process is necessary.
- Clinical Assessment: The first crucial step is a comprehensive medical history that includes a detailed account of the patient’s vasculitis symptoms, including their onset, duration, and accompanying symptoms.
- Laboratory Findings: The following blood and urine studies are crucial in the vasculitis diagnosis:
- Inflammatory Markers: Elevated C-reactive protein (CRP) and erythrocyte sedimentation rate (ESR) indicate inflammation in the body.
- Autoantibodies: The type of vasculitis can be identified by measuring specific autoantibodies, such as antinuclear antibodies (ANA), cryoglobulins, and ANCAs.
- Infectious Disease Screening: These are done to rule out infections that may be connected to vasculitis, such as hepatitis B and C.
- Organ Function Tests: It is crucial to perform the specific organ tests to assess liver, kidney, and other organ involvement.
- Imaging Tests: These imaging scans help visualize veins and arteries and assess involvement of organs:
- Angiography: X-rays of the arteries and veins shortly after injecting a contrasting dye can reveal narrowing, blockage, or aneurysm. There are several types of angiography, including conventional, CT, and MR angiography.
- Ultrasound: Can visualize larger veins and arteries and detect inflammation.
- PET scans: These can detect areas of swelling throughout the entire body.
- CT scan and MRI: Take sharp images of the inner parts to ascertain if there is swelling or damage.
- Biopsy: To pinpoint vasculitis, doctors perform a biopsy on the affected tissue (such as skin, nerve, kidney, or lung). This lets them examine the blood vessels under a microscope to identify the specific type.
Diagnosing vasculitis is not as easy as other tests; there are specific types of vasculitis that need a careful blend of clinical findings, lab results, imaging studies, and biopsy outcomes. Doctors often team up with other specialists to make sense of all this information.
Vasculitis Treatment
The main goals for treatment of vasculitis are to reduce inflammation, control the underlying autoimmune pathology, prevent organ damage, and move towards remission. Vasculitis treatment is individualized based on the subtype and severity of the vasculitis and the organs involved:
- Corticosteroids: Corticosteroids (e.g., prednisone) in high doses are typically the first line of therapy to achieve rapid reduction in inflammation. The dose is gradually tapered once the condition is improving.
- Immunosuppressants: These agents also serve to suppress an overactive immune response and are used in conjunction with corticosteroids, and/or they serve as a long-term maintenance therapy. Commonly used immunosuppressants include cyclophosphamide, methotrexate, azathioprine, mycophenolate mofetil, and rituximab.
- Biologics: There are some agents that are biologics that manipulate immune subsets such as B cells (e.g., rituximab) or interleukins (e.g., tocilizumab) that have been found to be particularly effective against some of the specific forms of vasculitis (e.g., ANCA-associated vasculitis or giant cell arteritis).
- Intravenous Immunoglobulin (IVIg): IVIg can be used in select presentations of vasculitis (e.g., Kawasaki disease and specific forms of small vessel vasculitis).
- Plasma Exchange (Plasmapheresis): Plasma exchange is a therapy that removes bad antibodies from circulation and is used in the setting of severe ANCA-associated vasculitis affecting the kidneys or lungs.
- Supportive Care: Symptom control and prevention of complications are essential. This could involve medication to control pain and blood pressure and infection prevention. Physical therapy and occupational therapy can assist in the preservation of mobility and function.
Vasculitis therapy is frequently long-term, necessitating close monitoring by a rheumatologist and other experts. The objective is to establish and sustain remission while reducing medication-related adverse effects.
When to Seek Medical Assistance?
One can seek assistance from a rheumatologist in the following cases:
- Worsening general symptoms
- Sudden onset of multiple, new, and unexplained symptoms
- New changes regarding skin and vital organs
- Numbness, tingling, or weakness
- Sudden vision changes & breathing difficulties
- Blood in urine or changes in urination
Conclusion
In conclusion, vasculitis is a complex and heterogeneous group of diseases that is primarily characterized by inflammation of the blood vessels. It is critical to recognize the wide range of vasculitis symptoms, understand the different vasculitis types and vasculitis causes, navigate a complex vasculitis diagnosis process, and implement individualized vasculitis treatment to lead to the best outcomes for patients.
Yashoda Hospitals provides comprehensive management of vasculitis via their specialization in rheumatology. We have specialists who can differentiate between types of vasculitis and describe the symptoms/conditions. Using diagnostic tests such as MRI, CT scan, or PET scan, the rheumatologists at Yashoda Hospitals can make an accurate diagnosis. Each patient with vasculitis is unique, and we develop individualized treatment plans to promote symptom relief and organ damage prevention. Treatment may consist of corticosteroids, immunosuppressants, and biologics. In addition, we introduce supportive therapy to help manage symptoms and prevent damage to organs. Yashoda Hospitals aims to provide effective management of vasculitis and promote better long-term outcomes for patients.
Have any questions or concerns about your health? We’re here to help! Call us at +918065906165 for expert advice and support.
















 Appointment
Appointment WhatsApp
WhatsApp Call
Call More
More